Acute Effect of a Single Session of Pilates on Blood Pressure and Cardiac Autonomic Control in Middle-Aged Adults With Hypertension
Article in The Journal of Strength and Conditioning Research · January 2019
DOI: 10.1519/JSC.0000000000003060
CITATIONS
8
READS
242
6 authors, including:
Jeferson Rocha
1 PUBLICATION 8 CITATIONS
Felipe Amorim Da Cunha
Rio de Janeiro State University
63 PUBLICATIONS 847 CITATIONS
Ricardo Cordeiro
Rio de Janeiro State University
9 PUBLICATIONS 38 CITATIONS
Walace Monteiro
Rio de Janeiro State University
132 PUBLICATIONS 2,357 CITATIONS
Some of the authors of this publication are also working on these related projects:
Doutoranda em Exercício físico e Esporte View project
Acute and chronic blood pressure responses to exercise View project
The user has requested enhancement of the downloaded file.
ACUTE EFFECT OF A SINGLE SESSION OF PILATES ON BLOOD PRESSURE AND CARDIAC AUTONOMIC CONTROL IN MIDDLE-AGED ADULTS WITH HYPERTENSION
JEFERSON ROCHA,1 FELIPE A. CUNHA,2 RICARDO CORDEIRO,1,3 WALACE MONTEIRO,1,2 LINDA S. PESCATELLO,4 AND PAULO FARINATTI1,2
1Graduate Program in Physical Activity Sciences, Salgado de Oliveira University, Nitero´i, Rio de Janeiro, Brazil; 2Laboratory of Physical Activity and Health Promotion, University of Rio de Janeiro State, Rio de Janeiro, Rio de Janeiro, Brazil; 3Esta´cio de Sa´ University, Cabo Frio, Rio de Janeiro, Brazil; and 4Department of Kinesiology, University of Connecticut, Storrs, Mansfield, CT
ABSTRACT
Rocha, J, Cunha, FA, Cordeiro, R, Monteiro, W, Pescatello, LS, and Farinatti, P. Acute effect of a single session of Pilates on blood pressure and cardiac autonomic control in middle-aged adults with hypertension. J Strength Cond Res XX(X): 000–000, 2019—We investigated the blood pressure (BP) and heart rate variability (HRV) responses to a single session of Pilates among adults with hypertension. Thirteen participants (7 women), aged 44–66 years, underwent Pilates and nonexercise control sessions separated by 48–72 hours in a randomized counterbalanced order. Blood pressure and HRV indices were simultaneously as- sessed 10 minutes before and 60 minutes after all sessions in the supine position: root mean square of successive differences (rMSSD), percentage of successive normal sinus RR intervals
.50 ms (pNN50), SD of all normal sinus RR intervals over 24 hours (SDNN), and low-frequency (LF) and high-frequency (HF) bands. After an acute session of Pilates, the mean values for area under the curve for systolic BP (p = 0.004, corresponding to 27.4 6 8.2 mm Hg) and mean arterial pressure (p = 0.023, correspond- ing to 25.3 6 5.4 mm Hg) were significantly lower compared to the control session. No significant difference was detected for diastolic BP (24.2 6 4.7 mm Hg, p = 0.106). Concomitant to BP reduction, significant lowering of parasympathetic HRV indi- ces occurred: RR intervals (264.1 6 69.9 ms$min21, p = 0.043),
rMSSD (28.3 6 15.4 ms$min21, p = 0.013), pNN50 (23.6 6
13%$min21, p = 0.028), and total power (23,089.4 6 5,938 m2$min21, p = 0.037). No difference was found for sym- pathetic markers: SDNN (217.7 6 34.6 ms$min21, p = 0.100),
LF (25.2 6 21,6 n.u.$min21, p = 0.417), and LF:HF ratio (20.3
6 5.2 ratio$min21, p = 0.422). In conclusion, a single session of Pilates reduced BP by ;5–8 mm Hg in adults with hypertension during the first 60 minutes of post-exercise recovery. Acute BP reduction was concomitant to lowered cardiac parasympathetic activity. Our findings are promising for the use of Pilates as an alternative exercise modality to lower BP.
INTRODUCTION
people with hypertension do not meet these recommenda- tions (26), and for about 20–25 of people, aerobic exercise does not lower blood pressure (BP) for reasons that are not clear (31). Thus, alternative exercise options for preventing, treating, and controlling hypertension are needed.urrent recommendations for adults with hyper- tension are to engage in moderate intensity aer- obic exercise supplemented by resistance exercise on most, if not all, days of the week (32). Yet, most
The Pilates method consists in a mind-body approach involving slow, controlled movements focusing on strength, posture, and breathing, which has become increasingly popular in recent years (11). Prior research examining health benefits of Pilates has mostly focused on quality of life (10), overall functional performance (4), and rehabilitation (22). However, there is a lack of studies about the hemodynamic effects of Pilates. On the other hand, current evidence indi- cates that isolate static/dynamic resistance exercise training is
capable to lower BP (6,23). Given the nature of Pilates, which
Address correspondence to Dr. Paulo Farinatti, paulofarinatti@labsau. org.
00(00)/1–10
Journal of Strength and Conditioning Research
© 2019 National Strength and Conditioning Association
largely applies strength exercises, it is possible to speculate that this modality might also induce favorable changes in BP. Sedentary middle-aged individuals are among those who most often seek the practice of Pilates (11). Therefore, chan- ces of finding people with high BP among the followers of
Post-exercise Hypotension and Pilates
this modality are high, which warrants research about its effectiveness as a supporting antihypertensive strategy. How- ever, we could find only 2 studies investigating the influence of chronic Pilates on BP—significant reductions were re-ported in healthy elderly (24) and hypertensive middle-aged
(25) women. Still, those studies did not examine the potential causes of chronic BP reduction. The antihypertensive benefits resulting from long-term exer- cise training are postulated to be for the most part the resultant from immediate, acute effects of a single exercise session, referred to as post-exercise hypotension (PEH) (21). This phenomenon has been reported after aerobic (8,12), resistance (23,36), and concurrent (18) exercise and may last for up to 24 hours after the exercise bout (see 30, Chap- ters 1 to 3, for a review). How- ever, to the best of our knowledge, no study has to date observed changes in BP after acute Pilates sessions.
Moreover, it has been sug- gested that PEH might relate to changes in the autonomic con- trol, particularly a decrease in sympathetic and increase in parasympathetic activity con- comitant with acute BP lower- ing (3,29). Nevertheless, other trials observed exactly the inverse (8,9,34,39). In short, it remains undefined whether autonomic changes contribute to PEH or only reflect a com- pensatory response to acute BP lowering. Regarding the poten- tial application of Pilates as adjuvant in the treatment of hypertension, it would be useful to know if acute changes in BP would relate to modifications in autonomic control, particularly in individuals with high BP.
Given these gaps in the liter- ature, this study investigated whether a single Pilates session would be capable to induce PEH among middle-aged adults with controlled hypertension. Further-
more, we verified the relationship between changes in BP and autonomic activity. We hypothesized that an acute reduction in BP would occur vs. nonexercise control sessions and that this would be related to changes in autonomic balance.
METHODS2. Journal of Strength and Conditioning Research
Experimental Approach to the Problem
Data collection included 3 visits to the laboratory. On the first visit, volunteers underwent clinical screening to confirm eligibility, and written consent was provided. Next, body mass and height were assessed, as well as BP, heart rate (HR), and HR variability (HRV) at rest. Subsequently, participants performed a familiarization session with basic Pilates exercises. On second and third visits, the individuals underwent either nonexercise control or Pilates sessions interspersed with 48–72 hours, in a randomized counterbal- anced order. Participants were told not to perform physical activities within 48 hours before the experimental sessions, to avoid caffeine and alcohol in the previous 24 hours, and to keep usual sleep and medication patterns. On arrival to the laboratory, BP and HRV were simultaneously assessed at rest. Variations of 5 in regard to values obtained on the first visit were accepted; otherwise, the participant should return another day (no case occurred). Heart rate was continuously assessed during Pilates sessions. Finally, BP and HRV were assessed each 10 minutes throughout 60 mi- nutes of post-exercise recovery. All procedures took place at the same hour of the day within each participant (always between 11 AM and 4 PM) to negate circadian effects, in a controlled temperature studio (22–258 C).
Subjects
Participants should be middle-aged (35–59 years), have prior diagnosis of hypertension by a physician, have no prior experience with Pilates, and be physically inactive (self- report) for at least 6 months. Additional exclusion criteria were cardiac or chronic kidney disease, stroke within the past
year, orthopedic problems compromising exercise perfor- mance, obesity, use of medication directly affecting autonomic activity (beta-blockers, amphetamines, and antidepressants), current smoker, and change of medication during research. After advertisement in social networks (Facebook, Twitter, etc.) and through explicative flyers, 68 individuals volunteered for the study. Of these, 54 were excluded due to predeter- mined criteria (diabetes = 9; orthopedic impairment = 4; smokers = 2; hypothyroidism = 2; use of beta-blockers = 4; use of antidepressants = 3; older than 59 years = 4; obese = 5; Pilates experience = 2; and no return = 19). During the exper- iment, another participant began to use beta-blocker and was excluded.
In short, data from 13 volunteers aged 45–65 years (7 women and 6 men) were analyzed (age: 54 6 5 years; body
mass: 77.6 6 11.7 kg; height: 166.7 6 9.1 cm; body mass
index 27.9 6 2.5 kg$m22; systolic BP [SBP]: 139.4 6
13.7 mm Hg; diastolic BP [DBP]: 84.6 6 9.5 mm Hg; and mean arterial pressure [MAP]: 103.4 6 10.6 mm Hg). Sub- ject characteristics were measured mean 6 SD. All partici- pants were on antihypertensive medication, whereas 4 used 2 or more drugs: angiotensin-converting enzyme inhibitor (n
= 3); diuretics (n = 1); beta-blocker + diuretics (n = 1); angiotensin II receptor type 1 (AT1) antagonist (n = 5); and AT1 receptor angiotensin II + diuretics (n = 3).
The experiment gained approval from institutional ethics committee (process 53949316.0.0000.5289). This study is part of a clinical trial registered at a WHO-accredited office (Brazilian Clinical Trials Registry [ReBec], protocol RBR- 93WPSF). Before enrolling in the study, all participants signed an informed consent form, as recommended by the Declaration of Helsinki.
| SBP (mm Hg) | 132.5 (13.9) | 130.6 (12.9) | 1.9 | 0.78 | 0.45 | 0.31 | 27.1 to 3.3 |
| DBP (mm Hg) | 80.3 (9.6) | 80.8 (10.4) | 0.5 | 0.24 | 0.81 | 0.09 | 24.0 to 5.0 |
| MAP (mm Hg) | 97.7 (10.7) | 97.5 (10.6) | 0.2 | 0.11 | 0.91 | 0.09 | 24.8 to 4.4 |
| HR (b$min21) | 68.0 (11.6) | 67.5 (8.8) | 0.5 | 0.24 | 0.81 | 0.04 | 24.7 to 3.8 |
| R-R interval (ms) | 875.7 (139.5) | 889.1 (98.1) | 13.3 | 0.49 | 0.63 | 0.09 | 246.1 to 72.7 |
| SDNN (ms) | 45.8 (18.1) | 48.8 (21.3) | 3.0 | 0.40 | 0.69 | 0.16 | 213.3 to 19.3 |
| rMSSD (ms) | 28.2 (16.8) | 28.7 (13) | 0.5 | 0.10 | 0.91 | 0.04 | 29.4 to 10.4 |
| pNN50 (%) | 10.4 (13) | 9.1 (8.5) | 1.3 | 0.43 | 0.67 | 0.17 | 28.1 to 5.4 |
| LF (n.u.) | 66.9 (19.8) | 71.3 (17.8) | 4.4 | 0.79 | 0.44 | 0.31 | 27.7 to 16.5 |
| HF (n.u.) | 32.9 (19.7) | 28.6 (17.7) | 4.3 | 0.78 | 0.44 | 0.31 | 216.4 to 7.7 |
| LF:HF ratio | 2.1 (0.8) | 2.5 (0.9) | 0.4 | 0.18 | 0.86 | 0.07 | 23.2 to 3.8 |
| Total power (ms2) | 2,486.2 (1913) | 2,633.2 (2,726.4) | 147.0 | 0.16 | 0.87 | 0.06 | 21888 to 2,182 |
 Post-exercise Hypotension and Pilates
Post-exercise Hypotension and Pilates
| Duration | HRmax | OMNI-RES | TRIMP | |
| Individual | (min) | (%) | Scale | (a.u.) |
| 1 | 48 | 57 | 3 | 3.0 |
| 2 | 52 | 61 | 4 | 7.7 |
| 3 | 59 | 53 | 4 | 3.2 |
| 4 | 55 | 61 | 5 | 3.7 |
| 5 | 55 | 66 | 3 | 6.4 |
| 6 | 65 | 55 | 3 | 3.5 |
| 7 | 62 | 53 | 4 | 4.3 |
| 8 | 55 | 55 | 4 | 4.0 |
| 9 | 48 | 55 | 3 | 3.8 |
| 10 | 48 | 62 | 3 | 8.9 |
| 11 | 57 | 61 | 4 | 9.5 |
| 12 | 50 | 65 | 3 | 4.2 |
| 13 | 48 | 50 | 3 | 3.2 |
Procedures
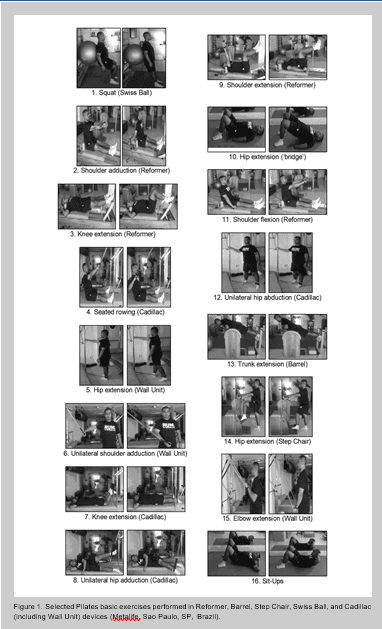
Pilates and Control Sessions. All Pilates sessions were ministered by the same trained instructor, using Reformer, Barrel, Step Chair, Swiss Ball, and Cadillac (including Wall Unit) devices (Metalife, Sao Paulo, SP, Brazil) and included: (a) warm-up including stretching and calisthenics for upper and lower body (8–10 minutes); and (b) Pilates exercises (basic) for the major muscle groups, as illustrated in Figure 1. A single set of 10 repetitions was performed for each exercise in a circuit format (approximately 50 minutes). Heart rate was continu- ously measured by a heart monitor, and the rate of perceived exertion was assessed after each exercise and at the end of the Pilates session, to maintain a constant intensity corresponding to scores 3–5 in the OMNI-RES Scale (27). The training impulse (TRIMP) in each session was calculated to assure that exercise intensity and volume were similar across subjects (2). TRIMP integrates in a single variable; both intensity and volume of training, being determined by multiplying the total duration of exercise bout (TD) by average heart rate reserve (HRR) as follows: (a) TRIMP, a.u. (men) = TD 3 HRR 3
0.64 3 e(1.92x HRR) and (b) TRIMP, a.u. (women) = TD 3 HRR 3 0.86 3 e(1.67x HRR). In the control session, subjects remained seated at rest during 60 minutes at the same local of Pilates sessions, to avoid bias due to environment.
Preparticipation Health Screening and Hemodynamic Assess- ments. As abovementioned, on the first visit participants underwent health screening including personal data, clinical status and medical history, medication use, and habitual physical activity levels within the past 2 months. Body mass was measured to the nearest 1 g by means of a digital scale, and height was measured in millimeter using a wall-mounted
stadiometer (Wiso, Guangdong, China). Subsequently, at-office BP and HRV were measured. Blood pressure assess- ment followed standard procedures (33). Participants remained in supine position during 10 minutes to stabilize BP and HR. After this, 5 BP measurements on the left arm were performed with 2-min intervals, by means of an oscillometric device (Om- ron 7,113; Omron Healthcare Co., Kyoto, Japan).
Heart rate variability was also recorded over 10 minutes at rest, using a cardiotachometer Polar RS800cx (Polar, Kem- pele, Finland). Data corresponding to 5-minute windows were extracted and downloaded for analysis by a specific software (Polar Precision Performance, Polar). Heart rate variability indices were analyzed using Kubios HRV software
 Figure 3. Mean (SD) HRV indices for 60 minutes into the recovery period after Pilates and control sessions (n = 13). p values indicate significant differences between Pilates vs. control (p , 0.05). HRV = heart rate variability; R-R interval = average of all normal R-R intervals; SDNN = standard deviation of R-R intervals; rMSSD = squared root of the mean squared differences of successive R-R intervals; pNN50 = percentage of successive R-R interval differences greater than 50 ms; LF = low-frequency band; HF = high-frequency band; LF:HF ratio = sympathovagal balance; DAUC = mean value for Pilates minus mean value for control within 60-minute recovery.
Figure 3. Mean (SD) HRV indices for 60 minutes into the recovery period after Pilates and control sessions (n = 13). p values indicate significant differences between Pilates vs. control (p , 0.05). HRV = heart rate variability; R-R interval = average of all normal R-R intervals; SDNN = standard deviation of R-R intervals; rMSSD = squared root of the mean squared differences of successive R-R intervals; pNN50 = percentage of successive R-R interval differences greater than 50 ms; LF = low-frequency band; HF = high-frequency band; LF:HF ratio = sympathovagal balance; DAUC = mean value for Pilates minus mean value for control within 60-minute recovery.
4. Journal of Strength and Conditioning Research
(Biomedical Signal Analysis Group, Department of Applied Physics, University of Kuopio, Kuopio, Finland), considering the last 5 minutes of recording. Sampling frequency was 1,000 Hz, and signal artifacts were filtered by excluding R-R intervals with differences of more than
20 vs. the preceding R-R interval. Filtering was per- formed in less than 1 of sequences for each subject. After Pilates and control sessions, BP and HRV were assessed each 10 minutes during 60 minutes of recovery, always in a supine position.
VOLUME 00 | NUMBER 00 | MONTH 2019 | 5
Post-exercise Hypotension and Pilates
Heart rate variability describes HR dynamics through measures in the time and frequency domains. Vagal-related HRV indices mostly reflect the magnitude of modulation in parasympathetic out- flow, as opposed to overall parasympa- thetic tone (37). In the time domain, the following vagal-related indices were ob- tained: mean R-R interval (R-R), SD of R-R intervals (SDNN), squared root of the mean squared differences of succes- sive R-R intervals (rMSSD), and percent- age of successive R-R interval differences greater than 50 ms (pNN50). These indi- ces are interpreted as markers of vagal dynamics within short periods (37). In the frequency domain, the power spec- trum was obtained with the fast Fourier transform method (Welch’s periodogram: 1,024 points, 50 overlap, and Hamming window). In this study, we have analyzed bands corresponding to low frequency (LF: 0.04–0.15 Hz), high frequency (HF: 0.15–0.40 Hz), and total power (TP; meaning LF plus HF). The LF:HF ratio was used to express sympathovagal bal- ance, as previously described (37). Spec- tral values were expressed as normalized units (n.u.), calculated by dividing the power of each component by the total variance from which the very LF compo- nent had been subtracted and multiplied by 100. This procedure increases the pre- cision of data regarding the relative con- tributions of LF and HF bands to total variability and autonomic balance (37).
Statistical Analyses
An achieved statistical power (1 2 b) of
0.85 was obtained by post hoc analysis using the software G*Power 3.1.5 (Uni- versitat Dusseldorf, Dusseldorf, Ger- many), considering n = 13, effect size = 0.8, and a = 0.05. Data normality was confirmed by the Shapiro-Wilk test, and thus, results are expressed as means 6 SDs. Cohen’s d effect sizes for mean dif- ferences were calculated and defined as small (0.20), moderate (0.50), and large (0.80). The Student t-test for paired sam- ples was used to test differences between BP and HRV values assessed before con- trol and experimental sessions. Overall, changes in BP and autonomic markers were expressed as areas under recovery
6. Journal of Strength and Conditioning Research
curves (AUCs), and differences between control vs. Pilates sessions were tested by paired t-tests. Associations between changes in BP and HRV indices were calculated by Pearson correlations. All statistical calculations were performed using the software SPSS 20.0 (SPSS Inc, Chicago, IL), and the probability level was fixed at p # 0.05 for statistical significance.
RESULTS
Table 1 shows data of hemodynamic and autonomic varia- bles assessed before control and Pilates sessions. The paired t-tests suggested that baseline values were similar across the experimental situations. Table 2 summarizes individual data in regard to intensity of Pilates sessions assessed through HR, RPE (OMNI-RES Scale), and TRIMP. The duration of Pilates sessions ranged from 48 to 65 minutes (mean 54 minutes). The intensity was moderate and quite similar across participants, corresponding to 50–66 of estimated maximal HR (mean 55 ) and OMNI scores between 3 and
- The overall volume as reflected by TRIMP ranged from 3
to 9.5 a.u. However, 7 of 13 individuals exhibited TRIMPs from 3 to 4 (;25 range), and 9 patients from 3 to 6.4 (;50 range). Only 2 participants exceeded this percent range.
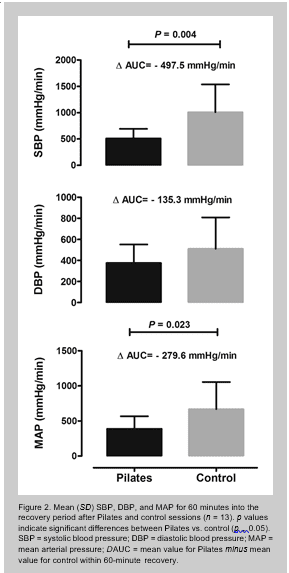
Figure 2 exhibits AUCs calculated for BP along the first
60 minutes after experimental sessions. As for SBP and MAP, AUCs were smaller after Pilates vs. nonexercise con- trol sessions. In comparison with nonexercise control ses- sions, SBP and MAP were lowered after Pilates by 27.4 6
8.2 mm Hg (i.e., ΔAUC [mean diff: 2497.5 mm Hg$min21; 95 CI: 2843.6 to 2151.3 mm Hg$min21; p = 0.004; Co- hen’s d effect size: 1.22]) and 25.3 6 5.4 mm Hg (i.e., ΔAUC [mean diff: 2279.6 mm Hg$min21; 95 CI: 2554.5 to 24.724 mm Hg$min21; p = 0.023; Cohen’s d effect size: 0.86]), respectively. However, DBP reduction (24.2 6
1.4 mm Hg, p = 0.106) did not achieve statistical significance. Heart rate variability data measured concomitantly to
BP are depicted in Figure 3. Albeit sympathovagal balance remained stable across conditions, parasympathetic markers as R-R interval (mean diff: 264.1 ms$min21; 95 CI: 2533.0 to 405.6 ms$min21; p = 0.043; Cohen’s d effect size: 0.73), rMSSD (mean diff: 28.3 ms$min21; 95 CI: 2776.7 to 256.7 ms$min21; p = 0.013; Cohen’s d effect size: 0.99), pNN50 (mean diff: 23.6$min21; 95 CI: 2532.9 to 10.07 $min21; p = 0.028; Cohen’s d effect size: 0.82), and TP (mean diff: 2133085 ms2$min21; 95 CI: 2281863 to 15694 ms2$min21; p = 0.037; Cohen’s d effect size: 0.76) were significantly lower after Pilates vs. control sessions.
Table 3 presents correlations calculated between changes in BP and autonomic markers. Significant and inverse corre- lations were found between changes in SBP and MAP vs. SDNN and TP. These predominantly parasympathetic indi- ces accounted for approximately 30 of BP variation.
DISCUSSION
The main purpose of this study was to determine whether a single session of Pilates compared with a control session would elicit PEH among adults with controlled hypertension. In addition, autonomic control as reflected by HRV was compared after Pilates and control sessions during the first 60 minutes of recovery. Systolic BP and MAP, but not DBP, decreased
;5–8 mm Hg within 60 minutes after exercise. This magnitude of BP reduction rivalled prior data resulting from aerobic and concurrent exercise (7,8,12,17). The immediate BP reduction after Pilates was concomitant to lowered parasympathetic activity (rMSSD and pNN50) and total HRV (R-R interval and TP). The present findings are suggestive that Pilates may be as effective antihypertensive therapy as aerobic exercise, albeit con- firmation in large samples is warranted.
In short, a single session of Pilates elicited significant PEH in middle-aged, sedentary, and hypertensive adults (Figure 2). These data provide promising preliminary insights into Pi- lates as a modality to be included in training programs pri- marily aiming at BP management. In practical terms, this is relevant because Pilates has become very popular among middle-aged adults who are not regularly engaged in other exercise modalities (11). Given the high prevalence of sed- entary behavior or low levels of physical activity exhibited by hypertensive patients (14), it is feasible to think that the Pilates method may be a useful long-term intervention for lowering BP.
Unfortunately, this question has been little investigated. We could find only 2 studies observing resting BP changes following chronic Pilates in individuals with high BP. Marinda et al. (24) showed that 8 weeks (3 nonconsecutive sessions per week, 60 minutes of duration, with increasing intensity) of Pilates produced a decrease of SBP (;7 mm Hg) in 25 prehypertensive elderly women. Martins-Meneses et al.
(25) demonstrated that 16 weeks of mat Pilates training (single sets of 5–10 repetitions in 12 exercises, 60-minute sessions per- formed twice a week) were capable to reduce SBP (;7 mm Hg), DBP (;3 mm Hg), and MAP (;4 mm Hg) assessed by ABPM-24 hour in hypertensive women. Evidently, to confirm the clinical utility of Pilates as antihypertensive therapy, further research is warranted. Moreover, although this study is sugges- tive that acute Pilates is capable to induce PEH, the role of successive BP reductions after acute Pilates sessions to produce long-term BP lowering must also be clarified.
The Pilates is a modality of training that combines static and dynamic resistance exercises, which are designed to improve muscle strength, flexibility, and balance. In general, the exercises are relatively easy for beginners and match the recommendations set forth by agencies as the American College of Sports Medicine (13). The Pilates exercises relate to what is known as the “5 essentials”—breathing, cervical align- ment, rib and scapular stabilization, pelvic mobility, and core strengthening (abdominal, gluteal, and paraspinal muscles). Ex- ercises to stabilize the core are essentially static, whereas muscle
VOLUME 00 | NUMBER 00 | MONTH 2019 | 7
conditioning involves dynamic contractions of high intensity, repeated a few times (19). In our case, the Pilates sessions consisted of a circuit including 16 basic exercises alternated by segment, performed with single sets of 10 repetitions (Fig- ure 1). All movements were performed dynamically but included static contractions at the end of their concentric phases.
Post-exercise Hypotension and Pilates
In a few words, our Pilates protocol combined exercises with dynamic and static components. In the absence of specific studies investigating the effects of acute Pilates on BP, the analysis of results from studies that described the hemodynamic responses to exercises performed with those types of contraction might help identifying potential simi- larities with our findings. Actually, few studies have inves- tigated BP after acute static or dynamic resistance exercises. Data from trials that applied acute static exercise are controversial. One trial reported a decrease in SBP of approximately 5 mm Hg (40), whereas others could not observe the same effect (15,28). On the other hand, PEH has been consistently detected after acute dynamic resistant exercise (1,18,36,39); the range of BP reduction in those studies was of 4–8 mm Hg, which is similar to our find- ings. Among the aspects that may explain this similarity, we highlight the fact that the present Pilates circuit included movements performed dynamically, albeit involving sus- tained static postures. Moreover, the exercises recruited large muscle groups, which is a major component of exercise volume. When considering the number of exercises, sets, and repetitions, the overall dynamic exercise volume in our protocol was therefore quite similar to what has been gen- erally applied by acute resistance exercise trials that suc- ceeded to observe PEH.
To the best of our knowledge, the autonomic responses after acute Pilates have not been so far investigated in individuals with high BP. One of the major determinants of PEH has been claimed to be the exercise pressor response (or ergoreflex), which is acknowledged to offset post-exercise sympathetic activity through muscle efferent stimulation (5,16). The ergoreflex contribution to lowered sympathetic modulation seems to be proportional to the amount of mus- cle work (5). Hence, exercises involving large muscle groups would more likely to induce PEH than those performed with small muscle mass, as demonstrated by previous research (20,35). Interestingly, in this study, BP reduction was parallel to a decrease in parasympathetic markers within the first hour of recovery, which does not agree with the premise that PEH would be due to increased vagal or low- ered sympathetic cardiac modulation during post-exercise recovery (5,16). Although contradicting the premise that changes in autonomic activity would be mechanisms under- lying PEH, it is worthy to notice that our data concur with those from other studies investigating BP and HRV re- sponses after acute resistance exercise. Rezk et al. (36) and Teixeira et al. (39), for instance, applied isolate resistance exercise sessions including 3 sets of 20 repetitions of 6
exercises performed with loads corresponding to 40 and
80 of 1RM (36) or 50 of 1RM (39). In both studies and regardless the exercise intensity, the PEH occurred parallel with a decrease in HF and increase in LF and LF/HF. More recently, Teixeira et al. (38) investigated the impact of acute isometric handgrip on BP and spontaneous cardiac barore- flex sensitivity. The spontaneous baroreflex increased during 10-minute post-exercise in men and during 30 minutes in women, along with total HRV power and RMSSD. How- ever, this greater cardiac vagal activity during recovery was concomitant to increased SBP, reinforcing the hypothesis that the BP behavior after acute resistance exercise is prob- ably dissociated from autonomic control.
The idea that PEH in this study was not mediated by changes in autonomic control is strengthened by the fact that HRV indices reflecting total autonomic activity, and particularly the parasympathetic branch (i.e., R-R interval, rMSSD, SDNN, pNN50, and TP), negatively correlated with changes in SBP and MAP. In fact, Table 3 indicates that BP tended to return to resting levels throughout the 60-minute recovery, whereas differences of TP and SDNN between Pilates and control sessions continued to increase. This ex- plains why D SDNN and D TP were inversely correlated with changes in D SBP and D MAP, suggesting that post- exercise decrease in BP was not concomitant to parasympa- thetic reactivation. These findings concur with the few previous studies that tested these correlations in prehyper- tensive and hypertensive patients following different exercise modalities, as treadmill walking (29), water-based cycle er- gometry, or land-based cycle ergometry (3). Further research is warranted to clarify whether this recovery pattern of car- diac autonomic activity might be related to a physiological reaction to offset the BP decline and to compensate for the resetting of baroreflex induced by the exercise pressor response.
Some limitations of this study must be acknowledged. First, type II error due to the small sample size may have occurred, particularly in regard to correlations between BP and autonomic changes after exercise. Moreover, a strict and individualized control of loads applied in Pilates is difficult due to the lack of springs’ resistance standardization. It is therefore impossible to ensure that all participants under- went the same stimuli in terms of muscle work. The lack of standardization of exercises across various Pilates meth- ods also makes it problematic to generalize our results to other situations in which the method is applied. Additional studies with different Pilates methods, applying different exercise volumes, and enrolling more experienced groups are needed to confirm our findings.
PRACTICAL APPLICATIONS
We have originally demonstrated that a single session of Pilates was capable to induce PEH during 60 minutes in hypertensive individuals under hypotensive medication. In addition, acute BP reduction was concomitant to lowered
8. Journal of Strength and Conditioning Research
parasympathetic activity. In practical terms, our results suggest that basic Pilates routines may induce acute BP lowering, which is useful information for practitioners. These findings are promising in regard to the application of the method as an adjunct strategy to antihypertensive therapy. However, further research with larger samples and pro- longed recovery is needed to ratify these initial findings. Moreover, the hypotensive potential of different Pilates methods should be investigated.
ACKNOWLEDGMENTS
This study was supported by grants from the Carlos Chagas Filho Foundation for the Research Support in Rio de Janeiro State (FAPERJ) and by the Brazilian Council for Techno- logical and Scientific Development (CNPq).
REFERENCES
- Anunciac¸ a˜o, PG, Poton, R, Szytko, A, and Polito, MD. Cardiovascular behavior after resistance exercise performed in different work ways and volume. Rev Bras Med Esporte 18: 117–121,
- Banister, EW, Morton, RH, and Fitz-Clarke, Dose/response effects of exercise modeled from training: Physical and biochemical measures. Ann Physiol Anthropol 11: 345–356, 1992.
- Bocalini, DS, Bergamin, M, Evangelista, AL, Rica, RL, Pontes, FLJ, Figueira, AJ, et al. Post-exercise hypotension and heart rate variability response after water- and land-ergometry exercise in hypertensive patients. PLoS One 12: e0180216,
- Bueno de Souza, RO, Marcon, LF, Arruda, ASF, Pontes Junior, FL, and Melo, RC. Effects of mat Pilates on physical functional performance of older adults: A meta-analysis of randomized controlled trials. Am J Phys Med Rehabil 97: 414–425,
- Chen, CY and Bonham, AC. Postexercise hypotension: Central mechanisms. Exerc Sport Sci Rev 38: 122–127,
- Cornelissen, VA and Smart, NA. Exercise training for blood pressure: A systematic review and meta-analysis. J Am Heart Assoc 2: e004473,
- Corso, LM, Macdonald, HV, Johnson, BT, Farinatti, P, Livingston, J, Zaleski, AL, et al. Is concurrent training efficacious antihypertensive therapy? A meta-analysis. Med Sci Sports Exerc 48: 2398–2406,
- Cunha, FA, Midgley, AW, Pescatello, L, Soares, PP, and Farinatti, Acute hypotensive response to continuous and accumulated isocaloric aerobic bouts. Int J Sports Med 37: 855–862, 2016.
- Cunha, FA, Midgley, AW, Soares, PP, and Farinatti, Postexercise hypotension after maximal short-term incremental exercise depends on exercise modality. Appl Physiol Nutr Metab 40: 605–614, 2015.
- de Oliveira, LC, de Oliveira, RG, and de Almeida Pires-Oliveira, Effects of Pilates on muscle strength, postural balance and quality of life of older adults: A randomized, controlled, clinical trial. J Physical Therapy Science 27: 871–876, 2015.
- de Souza, MvS and Vieira, CB. Who are the people looking for the Pilates method? J Bodyw Mov Ther 10: 328–334,
- Fonseca, GF, Farinatti, PTV, Midgley, AW, Ferreira, A, de Paula, T, Monteiro, WD, et Continuous and accumulated bouts of cycling matched by intensity and energy expenditure elicit similar acute blood pressure reductions in prehypertensive men. J Strength Cond Res 32: 857–866, 2018.
- Garber, CE, Blissmer, B, Deschenes, MR, Franklin, BA, Lamonte, MJ, Lee, IM, et al; American College of Sports Medicine Position Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor
fitness in apparently healthy adults: Guidance for prescribing exercise. Med Sci Sports Exerc 43: 1334–1359, 2011.
- Gerage, AM, Benedetti, TR, Farah, BQ, Santana, FdaS, Ohara, D, Andersen, LB, et al. Sedentary behavior and light physical activity are associated with brachial and central blood pressure in hypertensive PLoS One 10: e0146078, 2015.
- Goessler, K, Buys, R, and Cornelissen, Low-intensity isometric handgrip exercise has no transient effect on blood pressure in patients with coronary artery disease. J Am Soc Hypertens 10: 633– 639, 2016.
- Halliwill, JR, Buck, TM, Lacewell, AN, and Romero, SA. Postexercise hypotension and sustained postexercise vasodilatation: What happens after we exercise? Exp Physiol 98: 7–18,
- Keese, F, Farinatti, P, Pescatello, L, Cunha, FA, and Monteiro, WD. Aerobic exercise intensity influences hypotension following concurrent exercise sessions. Int J Sports Med 33: 148–153,
- Keese, F, Farinatti, P, Pescatello, L, and Monteiro, A comparison of the immediate effects of resistance, aerobic, and concurrent exercise on postexercise hypotension. J Strength Cond Res 25: 1429– 1436, 2011.
- Kloubec, J. How does it work and who needs it? Muscles Ligaments Tendons J 1: 61–66,
- Laterza, MC, de Matos, LD, Trombetta, IC, Braga, AM, Roveda, F, Alves, MJ, et Exercise training restores baroreflex sensitivity in never-treated hypertensive patients. Hypertension 49: 1298–1306,
2007.
- Liu, S, Goodman, J, Nolan, R, Lacombe, S, and Thomas, SG. Blood pressure responses to acute and chronic exercise are related in prehypertension. Med Sci Sports Exerc 44: 1644–1652,
- Lugo-Larcheveque, N, Pescatello, LS, Dugdale, TW, Veltri, DM, and Roberts, WO. Management of lower extremity malalignment during running with neuromuscular retraining of the proximal stabilizers. Curr Sports Med Rep 5: 137–140,
- MacDonald, HV, Johnson, BT, Huedo-Medina, TB, Livingston, J, Forsyth, KC, Kraemer, WJ, et al. Dynamic resistance training as stand-alone antihypertensive lifestyle therapy: A meta-analysis.
J Am Heart Assoc 5: e003231, 2016.
- Marinda, F, Magda, G, Ina, S, Brandon, S, Abel, T, and Ter Goon, D. Effects of a mat Pilates program on cardiometabolic parameters in elderly women. Pak J Med Sci 29: 500–504,
- Martins-Meneses, DT, Antunes, HK, de Oliveira, NR, and Medeiros,
- Mat Pilates training reduced clinical and ambulatory blood pressure in hypertensive women using antihypertensive medications. Int J Cardiol 179: 262–268, 2015.
- Mu, L, Cohen, AJ, and Mukamal, Prevalence and predictors of resistance and aerobic exercise among hypertensive adults in the United States. J Hum Hypertens 29: 394–395, 2015.
- Naclerio, F, Rodr´ıguez-Romo, G, Barriopedro-Moro, MI, Jime´nez, A, Alvar, BA, and Triplett, Control of resistance training intensity by the OMNI perceived exertion scale. J Strength Cond Res 25: 1879–1888, 2011.
- Olher Rdos, R, Bocalini, DS, Bacurau, RF, Rodriguez, D, Figueira, A Jr, Pontes, FL Jr, et al. Isometric handgrip does not elicit cardiovascular overload or post-exercise hypotension in hypertensive older Clin Interv Aging 8: 649–655, 2013.
- Park, S, Rink, LD, and Wallace, Accumulation of physical activity leads to a greater blood pressure reduction than a single continuous session, in prehypertension. J Hypertens 24: 1761–1770, 2006.
- Pescatello, Effects of Exercise on Hypertension: From Cells to Physiological Systems: New York, NY: Humana Press, 2015.
- Pescatello, LS and Kulikowich, JM. The aftereffects of dynamic exercise on ambulatory blood pressure. Med Sci Sports Exerc 33: 1855–1861,
VOLUME 00 | NUMBER 00 | MONTH 2019 | 9
Post-exercise Hypotension and Pilates
- Pescatello, LS, MacDonald, HV, Ash, GI, Lamberti, LM, Farquhar, WB, Arena, R, et al. Assessing the existing professional exercise recommendations for hypertension: A review and recommendations for future research Mayo Clin Proc 90: 801–812, 2015.
- Pickering, TG, Hall, JE, Appel, LJ, Falkner, BE, Graves, J, Hill, MN, et Recommendations for blood pressure measurement in humans and experimental animals: Part 1: Blood pressure measurement in humans: A statement for professionals from the subcommittee of professional and public education of the American Heart Association Council on high blood pressure research. Circulation 111: 697–716, 2005.
- Piepoli, M, Coats, AJ, Adamopoulos, S, Bernardi, L, Feng, YH, Conway, J, et al. Persistent peripheral vasodilation and sympathetic activity in hypotension after maximal exercise. J Appl Physiol 75: 1807–1814,
- Polito, MD and Farinatti, The effects of muscle mass and number of sets during resistance exercise on postexercise hypotension. J Strength Cond Res 23: 2351–2357, 2009.
- Rezk, CC, Marrache, RC, Tinucci, T, Mion, D Jr, and Forjaz, CL. Post-resistance exercise hypotension, hemodynamics, and heart rate variability: Influence of exercise Eur J Appl Physiol 98: 105– 112, 2006.
- Task-Force-of-the-European-Society-of-Cardiology-and-the-North- American-Society-of-Pacing-and-Electrophysiology. Heart rate variability: Standards of measurement, physiological interpretation and clinical use. Circulation 93: 1043–1065,
- Teixeira, AL, Ritti-Dias, R, Antonino, D, Bottaro, M, Millar, PJ, and Vianna, LC. Sex differences in cardiac baroreflex sensitivity after isometric handgrip exercise. Med Sci Sports Exerc 50: 770–777,
- Teixeira, L, Ritti-Dias, RM, Tinucci, T, Mion Junior, D, and Forjaz, CL. Post-concurrent exercise hemodynamics and cardiac autonomic Eur J Appl Physiol 111: 2069–2078, 2011.
- van Assche, T, Buys, R, de Jaeger, M, Coeckelberghs, E, and Cornelissen, One single bout of low-intensity isometric handgrip exercise reduces blood pressure in healthy pre- and hypertensive individuals. J Sports Med Phys Fitness 57: 469–475, 2017.



 Post-exercise Hypotension and Pilates
Post-exercise Hypotension and Pilates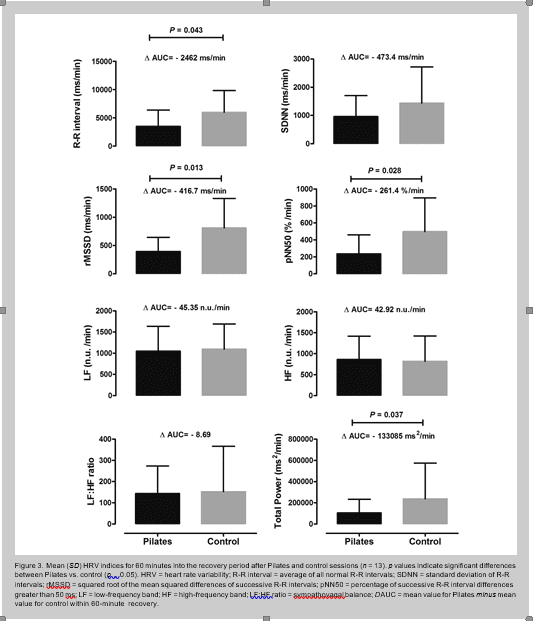 Figure 3. Mean (
Figure 3. Mean (

No comment